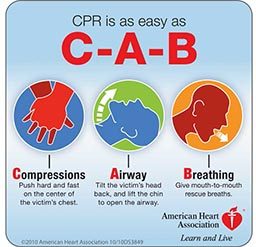
Every five years the International Liaison Committee on Resuscitation (ILCOR) announces revisions of CPR guidelines based on review of new scientific evidence. The current set of guidelines, published in 2010, established a major change in basic life support (BLS) techniques for cardiac arrest — from Airway, Breathing and Circulation (ABC) to Compressions, Airway and Breathing (CAB).1 These guidelines emphasize high-quality chest compressions, which means compressing the chest of an adult at least 2 inches (5 cm) at a rate of 100-120 times per minute while minimizing the period in which chest compressions are not being done to eight seconds or less.
In sudden cardiac arrest caused by irregular heart rhythms, the blood still contains several minutes worth of oxygen, and the immediate priority is to circulate blood and deliver that oxygen to the brain. Insufficiently trained rescuers often spend too much time not performing chest compressions, focusing excessively on ventilations or other tasks. In these situations, compressions alone will not restart the heart but are a temporizing measure to preserve as much as the brain as possible until an AED arrives to “shock” the heart back into a normal rhythm. To further emphasize the importance of circulating the existing oxygen in the blood, the current guidelines recommend that lay providers perform compression-only (“hands-only”) CPR until emergency medical services (EMS) or an automated external defibrillator (AED) arrives.
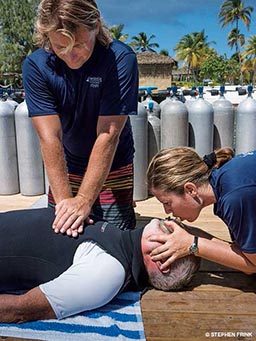
The ILCOR guidelines primarily address the most common and treatable types of sudden cardiac arrest: ventricular fibrillation and ventricular tachycardia. All other causes of cardiac arrest, including drowning, are considered special conditions and are covered by separate guidelines.2 These guidelines state that the most significant consequence of submersion is hypoxia and thus recommend that health-care-provider CPR employ a traditional ABC approach in submersion incidents. This is echoed in recent recommendations by drowning experts that providers follow a classic ABC approach, emphasizing the importance of rescue breaths.3 In light of these various messages, there is some confusion about how best to train lay providers in CPR. Another revision of the guidelines is expected in late 2015, but in the meantime, we ask the experts.
The 2010 guidelines changed the traditional ABC format to CAB. BLS protocols taught to health-care providers, however, still include the idea of using clinical judgment to decide whether to do compressions or ventilations first. This dilemma is especially present in case of drowning. Do you believe it makes a difference in patient outcomes?
Andrew Schmidt and Justin Sempsrott: To date, there is no good data to show that CAB or ABC is superior in the treatment of drowning patients. For the most part, the discussion about whether to do ABC or CAB for drowning patients is academic. In the past, a big focus was placed on the airway at the expense of chest compressions. The bottom line for health-care providers is that chest compressions should be performed at the correct rate and depth with minimal interruptions, and ventilations should be performed at the correct rate and volume. Whether the ventilations or compressions are initiated first, the other is delayed by less than 30 seconds. As long as the compressions are done well, it probably doesn’t matter which is done first.
Davut Savaser: When it comes to resuscitation I would recommend that everyone trained in BLS use the CAB algorithm. The beauty of an algorithm is that it is simple to follow — you have one task and one series of actions to complete; there are no alternatives.
Emphasis on bystander CPR (CPR by people with minimal training) has been moving toward compression-only CPR because it is easier to do and does not delay compressions with ventilation time. Do you think this approach helps or hurts in cases of cardiac arrest that result from drowning?
Schmidt and Sempsrott: Compression-only CPR administered by bystanders is applicable only to witnessed ventricular-fibrillation (VF) and ventricular-tachycardia (VT) arrests as a bridge to be used until an AED can be applied. Bystander CPR does not address drowning or any other causes of cardiac arrest. Compression-only CPR is not appropriate for drowning. In VF and VT, there is still oxygen in the blood after the heart has stopped. In drowning, the heart typically doesn’t stop beating until oxygen reserves in the blood are depleted. If a lay responder has no other training but is willing and able to perform chest compressions, they should do so regardless of the type of arrest.
Savaser: I think this helps in the context of drowning. The blood is carrying a certain amount of oxygen at the time cardiac arrest occurs, even if the arrest was the result of drowning. Compressions help by circulating blood (and whatever oxygen it’s carrying) throughout the body to perfuse vital organs such as the brain and heart. This is beneficial regardless of the cause of the arrest.
If there is only one bystander, I recommend compression-only CPR until additional help arrives. If there are two or more bystanders, I recommend performing compressions and ventilations concomitantly, prioritizing good compression technique (including adequate depth). CPR efficacy is maximized by alternating rescuers between each series of compressions and minimizing interruptions. Push hard and fast, folks!
High-quality CPR with minimal interruptions (less than eight seconds off the chest) has been shown to be a huge factor in resuscitations with favorable neurological outcomes. Does promoting ventilations by lay providers likely contribute to increased hands-off-the-chest time and thus decrease the likelihood of successful resuscitation?
Schmidt and Sempsrott: Guidelines for lay-responder CPR are meant only for the treatment of witnessed, out-of-hospital ventricular-fibrillation or ventricular-tachycardia arrests in adults. The goal is to circulate the oxygen already in the blood until an AED becomes available — ideally within the first four minutes. Continuous chest compressions in this specific patient population contribute to an increased chance of neurologically intact survival. In drowning, the cause of cardiac arrest is lack of oxygen, and lay-responder (compression-only) CPR does not apply. We encourage scuba divers, lifeguards, parents and anyone particularly likely to encounter a drowning person to take an advanced CPR course.
Savaser: High-quality compressions with minimal time off the chest are a crucial aspect of good CPR. As one performs repeated compressions, there is a build-up effect whereby perfusion increases to a higher level with each series of compressions. Longer intervals or pauses between compressions will decrease this buildup in perfusion and decrease overall efficacy of CPR.
One argument for teaching dive professionals traditional CPR instead of compression-only CPR is that they are more likely to encounter drowning victims who need ventilations. In your opinion, should we train dive professionals in either ABC or CAB resuscitation exclusively, regardless of whether the cardiorespiratory arrest occurred underwater or out of water?
Sempsrott: Lay-responder, compression-only CPR is applicable only to adults with witnessed ventricular-fibrillation and ventricular-tachycardia arrests as a bridge until an AED arrives. It would not be unreasonable for dive professionals to take CPR for health-care providers and for them to be capable of providing a higher level of care.
Increased distance to definitive care, complex medical problems such as decompression sickness, arterial gas embolism, drowning and marine envenomations all require more advanced treatment than what is taught in standard first aid and lay-responder CPR. Higher-level medical training can mean the difference between life and death for clients on a dive boat, whether it’s a liveaboard or a day trip. CPR for health-care providers and first-aid training specific to dive emergencies are layers of protection that help ensure personal and client safety. Buddy checks, safe diving practices, signaling devices, radios and medical training are just a few of the many ways safety is promoted. None of these is sufficient by itself, and none is useful without appropriate training.
Schmidt: CPR including ventilations administered by highly trained people does not equate to decreased survival in primary cardiac patients; compression-only CPR is primarily a technique for improving lay-person CPR. Thus, if the dive professional happens to do traditional CPR with ventilations on a cardiac patient, and they do it well, they are not harming the patient. In the context of water-based activities in which the etiology of arrest may be unclear, having the default treatment be traditional CPR with ventilations is probably a good protocol, assuming the staff has the appropriate training.
Savaser: I think the emphasis for both lay providers and health-care providers should be that compressions are the first line of intervention, followed by airway and breathing — as the CAB mnemonic illustrates. In the realm of BLS the type of arrest doesn’t matter — CPR via compressions, airway and breathing (CAB) applies. My opinion does not change based on remoteness or delay of access to higher care. CAB it, folks!
Our experts agree that in general, the efficiency of CPR depends on the timing and quality of chest compressions. Oxygenation and ventilation are important, but without quality chest compressions to circulate the oxygen, CPR is not effective. Thus, in bystander-witnessed cardiac arrests out of water, lay responders should apply compression-only CPR. Those with more advanced CPR training should follow the CAB approach. Cardiac arrest due to drowning, on the other hand, is caused by prolonged lack of oxygen, and restoration of breathing is very important. If the drowning person has not yet gone into cardiac arrest, initial rescue breaths may be lifesaving, and the classic ABC approach should be considered.
References
1. Field JM, et al. American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, Part 1. Executive Summary. Circulation, 2010; 122 [suppl]:S640-S656.
2. Vanden Hoek TL, et al. Part 12: Cardiac Arrest in Special Situations 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 2010; 122[suppl]:S829-S861.
3. Szpilman D, et al. Creating a drowning chain of survival. Resuscitation (2014). http://dx.doi.org/10.1016/j.resuscitation.2014.05.034
CPR for Drowning
“Cardiac arrest from drowning is due primarily to lack of oxygen. For this reason, it is important that CPR follow the traditional airway-breathing-circulation (ABC) sequence rather than the circulation-airway-breathing (CAB) sequence, starting with five initial rescue breaths, followed by 30 chest compressions, and continuing with two rescue breaths and 30 compressions until signs of life reappear, the rescuer becomes exhausted or advanced life support becomes available.
In cases of drowning, the European Resuscitation Council recommends five initial rescue breaths instead of two because the initial ventilations can be more difficult to achieve, since water in the airways can interfere with effective alveolar expansion. CPR with chest compression only is not advised in persons who have drowned.”
Source: Szpilmann D, et al. Drowning. N Engl J Med 2012; 366:2102-10.
Meet the Experts
Davut Savaser, M.D., MPH, is board certified in emergency medicine and undersea and hyperbaric medicine. He is a faculty member in hyperbaric medicine and the emergency department at the University of California, San Diego, Hospital System. Dr. Savaser, a DAN attending physician, also works with EMS in the San Diego area.
Andrew Schmidt, D.O., MPH, is assistant clinical professor of emergency medicine at the University of Florida College of Medicine–Jacksonville and a co-founder of Lifeguards Without Borders. Dr. Schmidt has assisted with establishing lifeguard programs all over the world and has lectured on drowning at conferences including the World Congress on Drowning and EMS World Expo.
Justin Sempsrott, M.D., is a co-founder of Lifeguards Without Borders and an emergency medicine physician practicing in Lexington, N.C. He serves as medical director for Starfish Aquatics Institute and for several EMS agencies in North Carolina. Dr. Sempsrott has assisted with establishing lifeguard programs and has lectured on drowning all over the world.
© Alert Diver — Q1 Winter 2015